General medicine case -2
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based input.
Date of admission : 18/12/2021
A 20 year old male patient presented to the OPD with the chief complaints of low grade fever ,vomitings and weakness since 3 months
HISTORY OF PRESENT ILLNESS:
patient was apparently normal 3 months back then he developed low grade fever and vomitings 2- 3 episodes per day and he visited local hospital 2 months ago they suggested for a blood test and was told that there is increase in bilirubin levels and decreased in haemoglobin and there he got admitted for a day and went back to his home and referred to an ayurvedic doctor to control his bilirubin levels they gave herbal medicine which he continued for a month. And went for routine check up for every 15 days there is fall in haemoglobin levels where they suggested for blood transfusion and then he visited our hospital
no similar complaints in the past
Patient is not a k/c/o diabetes , hypertension,asthma , tuberculosis, epilepsy
No surgeries in the past
PERSONAL HISTORY:
appetite : lost since 3 months
Bowel : irregular (alternate days )
Micturition: normal
Diet : mixed
Habits : alocholic since 6 - 7 years back ( one beer daily) and stopped a year back
Smoking since 6-7 years back (1-2 ciggerates per day ) and stopped an year back
Sleep : adequate
FAMILY HISTORY:
no similar complaints in the family
GENERAL EXAMINATION:
patient is conscious , coherent, cooperative
Pallor - present
Cyanosis- absent
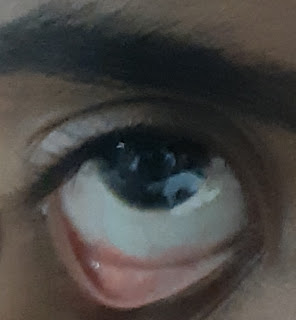
Icterus- present
No lymphadenopathy
Malnutrition: absent
Clubbing - absent
BP : 120/70 mmHg
Pulse rate : 92 beats per min
Respiratory rate : 18 cycles/min
Spo2 at room temperature: 98%
Systemic examination:
CNS :
Patient is Conscious
Speech normal
Cranial nerves : intact
CVS :
S1 , S2 sounds heart
No murmers
RESPIRATORY SYSTEM:
Position of trachea- central
No vesicular breath sounds heard
PER ABDOMEN:
No tenderness, palpable mass
Liver and spleen not palpable
INVESTIGATIONS :
PROVISIONAL DIAGNOSIS :
Hemolytic Anemia with jaundice
DIFFERENTIAL DIAGNOSIS:
Megaloblastic anemia ,
FINAL DIAGNOSIS:
Pancytopenia
TREATMENT:
-INJ vitamin b12 (NERVIGEN ) 100MG IN 100ML NS /IV STAT
- TAB OROFER -XT PO/OD
- TAB MVT PO /OD
-BP , TEMPERATURE, PULSE RATE MONITORING EVERY 4 HOURLY

















Comments
Post a Comment